Following recent events regarding the detention of the ex-deputy minister of health and ten doctors in the case of manipulations with the transplantation system in Ukraine, society is concerned and interested in an honest review of the functioning of this important medical field. In order to understand the real situation, we turned to an outstanding figure in this direction, Vasyl Strilka, who is respectfully called the "father" of transplantation in Ukraine.
Back in 2020, when we wrote about the first bone marrow transplant for a child in Ukraine from a non-family donor, the arrows led to Strelka - as a person who strongly intervened to make this possible by law. Currently, Mr. Vasyl heads the Directorate of High-tech Medical Care and Innovations at the Ministry of Health.
Where do organs for transplant come from?
"Transplantation is impossible if there is no donor organ," begins Vasyl Strilka. That is, there must be a donor who is diagnosed with brain death, but whose heart is still beating.
The brain can die due to various reasons. For example, a road accident. Or a stroke. According to foreign scientific data, Vasyl adds, about 50% of those who die as a result of a stroke go through the stage of brain death.
In Ukraine, 130,000 Ukrainians have a stroke every year, more than 25,000 of them die. And the numbers are growing.
Brain death is diagnosed in intensive care and intensive care units. And this, says Vasyl, is the main problem of the system. After all, until the council of doctors meets and confirms this diagnosis, there is no question of a person who is actually already dead becoming an organ donor for other living people.
According to the order of the Ministry of Health, which was copied from the European and American ones, the diagnosis of brain death must be made for all patients who have three points on the Glasgow coma scale. Even if it is an old grandfather. But in practice it is not like that.
"I graduated from Bogomolets Medical University in 2012. During my entire education, I was not told anything about brain death, its diagnosis, that such a diagnosis exists. And tens of thousands of such doctors were released. They work. When something occurs to you that you have not done before, you think: do I need it? In May 2019, representatives of the WHO, who were key at that time in transplantation, came to us. I ask one, a Spaniard: "Tell me what you do so that your doctors diagnose brain death?". He did not understand the question: "So? This is their duty." They do not understand our problem. Ours is precisely in intensive care and intensive care units," emphasizes Strelka.
He recalls that in 2019 there were almost 0 such diagnoses, only in the Zaporizhzhia region something was done, one or two people a year became organ donors there. Kidneys were removed for transplantation, several posthumous kidney transplants were performed throughout Ukraine.
And five years later, there are few brain death diagnoses in the country. Because, in addition to the directive order, there must also be the desire of doctors and equipment for this.
One doctor said off the record that sometimes, in order to diagnose brain death in a regional hospital, a team of specialists from the transplant center went there with their equipment: ultrasound, gas analyzer, and so on.
It is important that these are not transplant specialists, but anesthesiologists or neurologists, for example.
The arrow confirms that such a problem exists. What's more, the equipment for such diagnostics should already be in intensive care units and intensive care units, he adds. For example, the same blood gas analyzer to treat patients who get there.
There is also a corresponding order of the Ministry of Health that all this equipment must be there and, if necessary, used for the diagnosis of brain death.
"Is it everywhere? Differently. I would like to be treated in a unit that diagnoses brain death or performs transplants. Because in this case, my chances of survival are higher, because the qualifications of the doctors there are higher. They not only have the equipment, but also use it," explains Vasyl Strilka.
All intensive care units and intensive care units should routinely be able to diagnose brain death themselves. But the reality is not like that. It is often difficult for railcars to start something - because of fear and ignorance, he adds: "That's why it's normal and good to have someone help you get started."
And here we come to an interesting and ethically debatable decision of the Ministry of Health in medical circles — cooperation agreements between hospitals that are transplant centers and hospitals that are potential extraction bases, that is, where there is an intensive care unit and the ability to diagnose brain death.
Whoever is more active will get more organs
In order for a transplant center to do a transplant, save its patient, and get good money from the state for it, it needs organs.
They can appear only when the resuscitation and intensive care units diagnose brain death. Of course, only some of them will be suitable for donation, but it is no longer 0.
Therefore, the Ministry of Health made sure that transplant centers were interested in training local hospitals. For this purpose, cooperation agreements were foreseen in 2021, since transplantation is "team work, which usually involves several hospitals; The Ministry of Health has drawn up rules to encourage interaction and cooperation between hospitals."
If a transplant center contracts with a local hospital, teaches it, perhaps even shares equipment, it gets priority rights to the organs that will appear there as a result of the death of patients.
In off-the-record conversations, doctors involved in transplantation explained that, in particular, this is how the bias appeared in the country: some transplant centers quickly visited many hospitals, signed contracts with them, and now receive the lion's share of organs. It's a kind of principle that whoever jumps up faster gets the slippers.
Many contracts were signed, in particular, by the Shalimov Institute, the Heart Institute and the First Territorial Medical Association of Lviv. According to the statistics of previous years, they are leaders in the number of organ transplants.
What is the solution to the problem and the ethical dilemma at the same time? The fact is that in Ukraine at the same time there is and is not a single waiting list for organs.

Each transplant center has its own list, already installed in the general electronic system of EDIST, which we will talk about later.
A patient from a center with many contracts has a higher chance of receiving an organ in time, another may die without waiting. Thus, patients with the same indications for transplantation find themselves in unequal conditions.
On the one hand, such rules push the system to develop. On the other hand, the patient is not to blame for the fact that his center did not sign many contracts. There were doctors who did not believe that their patients from less active centers would survive the transplants.
Vasyl Strilka answers that this is not a question of faith, but of the work of doctors with other hospitals. In addition, the system gives first priority to emergency patients who can die without a transplant in a matter of days, outside of all contracts, looking for donors for such people throughout the country.
"In 2018, we had four or five transplant centers that performed only family kidney and liver transplants, and in Zaporizhzhia they performed a couple of kidney transplants from a posthumous donor. That is, we had people who did transplants. But they did not show activity, while saying that they wanted to save people. The Verkhovna Rada passed a law that gave impetus to the system. And the rules that one must visit hospitals are an order of the Ministry of Health. They were told about transplantation, the stories of patients who need transplants. This is a couple of thousand people. Because for some adequate period there is no other way to develop the system."
He adds that those transplantation centers that are more stressed, visit hospitals, give them advice, and as a result, more organs are transplanted. That is why there is a discrepancy that some do 100 transplants a year, while others do two to five: "We see that cooperation between transplant centers and hospitals increases the level of donation."
He also says that one hospital can now have several contracts with transplant centers. Even with everyone.
Last year, transplants were made in 26 centers. And in total, about 40 contracts were concluded with NSZU for this.
"There are 12 hospitals that have a stroke center, contracts with the NHSSU for transplantation, and did not perform transplants in 2023," says Strilka. And he adds: if they continue like this, the state will not conclude contracts with them for transplants in 2025.
Instead, those centers that perform transplants are becoming more specialized, it is better for patients to go there, because the chances of receiving a donor organ are higher.
Regarding the centers that do not have so many transplants and contracts, Mr. Vasyl says the following: there are regional hospitals and stroke centers in Ukraine that have not yet implemented routine diagnosis of brain death. You can send your specialists there, sign agreements and increase transfers.
After all, now the Ukrainian system covers about 10% of the real need, Strelka points out. And compares Ukraine with other leading states in terms of the number of transplants. In the world, this indicator is calculated by the number of transplants per million population. In 2023, Ukraine held:
- 61 heart transplants: if we were at the level of Croatia, we would transplant 440 hearts;
- 4 lung transplants: if we compare with Austria, we should have 505 such transplants;
- 243 kidneys: if we compare with the leader - Spain, then there should be 2500 kidney transplants per year.
Currently, there are 3.6 posthumous donors per million population in Ukraine. If you do not count the two or three donors per year who were in Zaporizhzhia, the country had 0. But Spain has an indicator of more than 40, the USA - more than 40. The average indicator for Europe is 25-40. That is, it is possible to increase the Ukrainian system by 10 times, argues Vasyl.
How the brain death diagnosis algorithm and organ removal permits work
Let's move on to another important component of the system — the work of the transplantation algorithm itself.
When a patient in the intensive care unit has three points on the Glasgow coma scale, a council of doctors meets and diagnoses brain death.
According to Strelka, this is a simple procedure, all the necessary skills were taught at the medical university, it's just that they didn't explain that there is such a diagnosis.
It is necessary, for example, to check reflexes, do an apnea test (temporary cessation of breathing), electroencephalography (shows whether there is electrical activity in the brain), and so on.
Vasyl Strilka says that such a diagnosis cannot be wrong: "If the study shows that there is no blood flow in the brain, then it is not there. Each doctor checks his own, goes through the checklist defined by the Ministry of Health."
If the hospital has a cooperation agreement with the transplant center, it can help with diagnosis. For example, to send their intensive care specialists, but not transplant specialists, to consult remotely, to watch online analyzes and indicators, to advise somewhere to adjust the drugs so that the heart does not stop, because then there will be no transplant.
Brain death is diagnosed without reference to transplantation, Strelka emphasizes. After all, studies say: if this diagnosis is tied to transplants, the level of donation becomes small. Like, then doctors can decide by eye: "Maybe this will be a donor? But no," and not even to carry out diagnostics.
After the council of doctors has declared brain death, doctors check whether the deceased person has contraindications to donation. For example, infectious diseases.
If there are contraindications, according to the order of the Ministry of Health, life support should be stopped. That is, you need to turn off the ventilator.
"This is also about human dignity. Because we were told about cases when a stroke was treated in the intensive care unit, the person already had brain death, which was not officially diagnosed, and the relatives of the already deceased were sent to the pharmacy every day to buy thousands of hryvnias worth of medicine. This should not be the case. No one has yet been resurrected after brain death," says Strelka.
And he adds that after the diagnosis of brain death, a person is considered dead according to the law. After all, biological death is irreversible.
Certificate. Article 52. Determination of irreversible death of a person and cessation of active measures to support the patient's life. Medical workers are obliged to provide full medical care to a patient in an emergency. Active measures to support the patient's life are stopped if the person's condition is determined to be irreversible. The moment of irreversible death of a person is the moment of his brain death or his biological death.
If a person has no contraindications after the diagnosis of brain death, he is considered a potential donor. At this stage, the transplant coordinators of the hospital where the donor is, or the Ukrainian Transplant Coordination Center, are included. He is responsible for coordinating the entire system.
If a donor appears, the transplant coordinator of the hospital where the donor is located communicates with relatives about consent to organ removal, organizes all the necessary research and enters data into EDIST. The transplant coordinator of the Ukrainian Transplant Coordination Center provides support for the distribution process through EDIST according to the rules of the Ministry of Health.
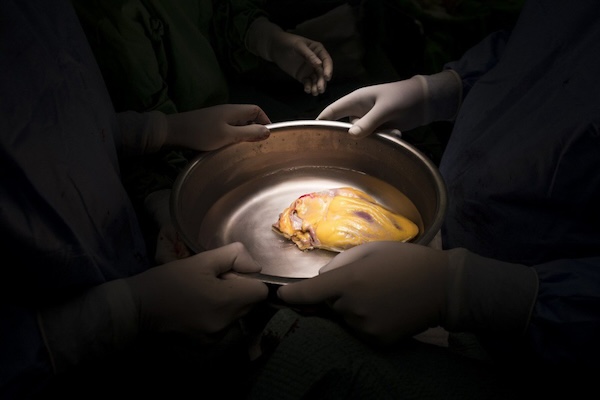
If the relatives have given their consent to the removal of organs, the donor undergoes additional examinations, and only then the automated system selects potential recipients of the organs that the relatives have agreed to donate. For example, they may allow removal of the liver and kidneys, but not the heart.
How the system chooses who gets a particular organ: the transplant waiting list
First, the algorithm looks for whether there are patients throughout Ukraine who have an emergency status for a transplant. That is, if these people do not have an organ for transplantation in the coming days, they will die. No contracts between hospitals are relevant here.
If there is such a person and she is basically compatible in terms of blood group and anthropometric data (a 50-year-old kidney will not fit a 6-year-old child), the system first of all offers the organ to her.
The transplant coordinator of the transplant center checks what is with her now and informs the Ukrainian Transplant Coordination Center about it. Because yesterday a person could be alive, today, unfortunately, no longer.
Additional studies are next. For example, a cross-match: the blood of the donor and recipient of the organ are checked for compatibility.
If everything is ok and the transplant doctors decide to operate, they plan a transplant. If there is no emergency recipient, i.e. a person who urgently needs a donor organ, or something is not suitable, the system searches further. Checks whether the extraction base has a cooperation agreement with any transplant center.
If it has, it first looks for recipients of the organ there, whether there are any matches. If the hospital has several contracts with transplant centers, it searches among several waiting lists.
Can one person wait in line at multiple transplant centers to increase their chances of getting a transplant?
Strelka explains that no: “If a person needs a transplant, he is very sick. For example, the heart works very poorly. Someone should deal with such a person. If she had stood in three centers in a row, we would not have found the extreme later."
If the hospital does not have a contract with any transplant center, the system searches immediately across the country.
When there are several people who are potentially suitable for a particular organ, the system checks which of them is longest in the queue, who has given lifelong consent to the removal of organs in the event of their death.
"This is also taken into account. So I gave lifelong consent, and someone did not. All other criteria are the same for us. It is fairer to give the organ to me, because I was ready to give mine to someone," Strelka explains.
And so he forms a waiting list of those whose basic indicators are suitable for an organ that has not yet been removed, but has already received consent for it from relatives.
Then the doctors take the stage. The center that is higher on the list can agree to take the organ or refuse it, and this is how it happens in the world.
"In the US, every organ, even, in someone's opinion, not very, will be offered to all transplant centers until the last one refuses," says Strelka. — Colleagues from the USA told about a case of lung transplantation. All centers on the list began to refuse them, because the donor had partial pneumonia. While the centers refused, three days passed, the doctors who supported the body cured the pneumonia, and the last center on the list took a healthy lung for transplantation.
Why can doctors refuse organs? For example, says Vasyl Strilka, a 20-year-old boy is waiting for a heart transplant. He is not in the first emergency status, the projected length of his life is at least a few more months.
And the donor who appeared in the system and suits him is 59 years old. According to the indicators, this heart can be suitable for a 20-year-old, but transplant specialists will think whether it is worth transplanting an old heart to a young one. Maybe it's better to wait for another one that will work longer.
Or there may be a 70-year-old man who is lower in the waiting list due to age, but a 59-year-old heart will suit him perfectly.
Or in another way: the 20-year-old boy is already in the first emergency status, the expected life expectancy is a week. That is, he will either die or get a 59-year-old heart. In this case, doctors will transplant it, let the heart live not for 15 years and then there will be a retransplantation, but for four or five. And for the boy, this is not only a chance to live these years, but also a chance for retransplantation.
Is it possible to abuse doctors here? When the patients higher on the list are not called, but note that they refused, or are sick, or abroad, etc., then the organ is received "by agreement". Vasyl Strelka answers that the patient may not be called, he may have contraindications right now, he can refuse the transplant right now:
"In any case, such cases are recorded on paper with the signature of the responsible person, which makes it possible to find out. The final selection of the recipient takes place on the basis of the results of the immunological test for compatibility, these results are also documented."
Can doctors, transplant coordinators, somehow enter data into the system so that certain organs receive specific centers? The doctors assumed in the conversations that the problems were allegedly probable precisely at the stage of the human factor before entering data into YEDIST. Because technically, all interlocutors had no questions about YEDIST, the automated system was praised.
As an example, one interlocutor cited Germany, where cases of such conspiracies were allegedly proven. When the patient's clinical data were changed so that he became an emergency just before the appearance of the desired donor organ in the system. Conventionally, the transplant center changes the data in the system so that their patient acquires emergency status, and then the transplant coordinator enters the donor data - and the system automatically combines them.
"If this was the case in Germany, theoretically it could be here as well," says Strelka. — But due to the formalization of relations and consideration of cooperation between the transplant center and the extraction base, we reduce the likelihood of such things. Because the transplant center understands that the organ will most likely come to them anyway according to the contract. This reduces the incentive to somehow play. For four years, we had fewer emergency statuses and they were more streamlined. Therefore, in 2021, we wrote out the criteria for emergency statuses. For example, a patient in the first cardiac status should already be on ECMO." When the heart and lungs are supported artificially, the person is still alive.
How well are organs transplanted in Ukraine?
Some doctors pointed out that supposedly weaker teams can perform transplants, because their management strained and signed contracts, and centers with stronger specialized teams for some organ practically do not operate.
"This is a complex story," replies Vasyl Strilka. — The first (after a 15-year break) heart transplantation in Ukraine took place in the Kovel district hospital. Has she ever had a transplant? No. Was there anyone to do it? No. Manager Oleg Samchuk wanted to - and they did everything necessary. Brain death diagnosis was launched there.
When a donor appeared there, they invited Boris Todurov (who was once the first to transplant a heart in Ukraine) to do the transplant. The team was already standing next to him and studying, in particular Roman Domashich, who is already undergoing a heart transplant in Lviv. Then the time came when they realized that they could do it themselves.
This is already the case not only with Boris Todurov, but with up to a dozen cardiac surgeons who have transplanted a heart at least once. This is how we do professional demonopolization, increasing the pool of those who are able to do it, and a person can have a choice."
We need three to five centers that can transplant a specific organ in order not to be dependent on one manager, adds Vasyl Strilka. There are already six liver transplantation teams: "Feofania", two teams at the Shalimov Institute, Okhmatdyt, Lviv Territorial Medical Association, "Oberig".
"If the head of the institution is interested in transplantation, he will lure good transplantologists to work - at a quarter, half rate.
When there are several people who are potentially suitable for a particular organ, the system checks which of them is longest in the queue, who has given lifelong consent to the removal of organs in the event of their death.
The state pays well for transplantation. This allows not to take money from the patient. When calculating the tariff, we told transplant centers: calculate so that you do not have to take money from patients in any case.
So that you can pay a normal salary to the team. And at the same time, the state saves a million hryvnias on each kidney transplant compared to what we used to pay Belarusians (under the program of treatment abroad). We also save more than a million on heart transplantation. In addition, transplantation raises the level of the entire hospital. She then needs to train her laboratory, cardiologists, and anesthesiologists."
I am asking about the Kyiv case, which the doctors told off the record. When they sent a team of transplant specialists to the States for training, they trained, they brought them - and they do not transplant. Vasyl Strilka says that the team was sent to the USA because there was a problem - no one transplanted lungs on the territory of Ukraine.
The first lung transplant was performed in Lviv when Polish doctors arrived and performed it together with local people. The people of Lviv have already made the second one themselves. But one of the team went to work in Poland.

Later, Vasyl Strilka met a cardiac surgeon, a transplant specialist of Ukrainian origin Serhii Melnychuk, who works at Mass General Hospital. This is a world-class hospital. One of the clinical bases of the Harvard Medical School. Melnychuk helped get her to agree to teach lung transplants to 13 doctors from Ukraine. The basis of the team - 11 doctors - were from "Feofania", two more cardiac surgeons - from other institutions.
The Christian Medical Association helped with accommodation and logistics. The team spent three months there. She studied and upon her return independently performed several lung transplants in Ukraine.
But again the narrowest point of the Ukrainian system, Strilka says. Transplanting a lung is more difficult than a heart, kidney or liver. After all, the lungs have contact with the external environment. And if there is an infection in the hospital that carries out the transplant, then against the background of immunosuppression (suppression of immunity, which is done to the patient artificially so that the body does not reject the transplanted organ), this infection progresses and the person has a high risk of dying.
"For the lungs to be suitable for transplantation, the donor must be from a very good intensive care unit," Vasyl explains. - From the one where they treat very well. Then there is a higher probability that, in case of diagnosis of brain death, the patient will have lungs suitable for transplantation. Very few hospitals can treat patients who will either recover or have brain death and have usable lungs in this way. The people of Lviv were able to perform a lung transplant, because they have a well-established work in intensive care."
"Feofania" is currently receiving many casualties as a result of combat, and this also takes away the resource of teams and equipment. Therefore, the question is not for trained doctors, says Strelka, but for several factors: "Because you can transplant lungs, but in the next ward there will be a patient with some kind of resistant microflora (that is, an intra-hospital infection, where there will be bacteria that are not affected by antibiotics) and because of immunosuppression a person will not survive."
In various hospitals, it is precisely because of nosocomial infections that people who receive transplants sometimes do not survive. First Deputy Minister of Health Serhiy Dubrov spoke earlier about the spread of such serious infections that are resistant to antibiotics.
And here we come to the last important issue of the system — the survival rate of Ukrainians after transplants.
Several doctors said off the record that teams with better transplant skills and higher survival rates transplant fewer organs than hospitals that have contracts and transplant more organs.
In their opinion, this is unfair even to a patient who should be operated on by the best specialists and who should know in which hospital the risks of survival or death are higher. There are no publicly available statistics.
"Currently there is no. Someday it will be," Strelka replies. He says survival figures will not be released at this time:
"On average, our indicators are a little worse than the average European ones. If we look at the hospitals that performed three or four transplants on serious patients due to the emergency status, and two of them died, the system will not be appreciated here. To publish statistics, it is necessary to show a breakdown by each center.
If one center performed three transplants on three severe patients, one of whom died, the survival rate would be 67%. Is it good or bad? And someone who has had 100 transplants will have a 90% survival rate. And then no one will go to the center where there were three patients.
But 67% of them are not because their hands are crooked, but because there are still no adequate numbers for evaluation.
There is another side of the coin.
Can any action be taken against centers with worse survival rates? Some countries publish such indicators. And there, difficult patients have almost no chance of transplantation. Because no one wants to take them, as they will spoil the statistics.
Because a serious patient has a 70% chance of dying and not surviving after transplantation. And they play him.
We are only at the stage of formation: if we do this, the centers will not accept patients who could survive. Internally, we show the data to the centers, but publicly at the moment it would rather be a detriment to the transplant system. The words that some have worse results and more transplants, and some have fewer and better results, are not supported by anything. We see that centers that do more transplants have better results.
This is due to several factors:
– they gain experience; even if someone was very smart but did two transplants, and someone worked hard and did 40, then I would go to someone who did 40. The best heart transplant result is now at the Heart Institute. They all live from the last 21 transplants;
– we still need more transplant teams; if they say that the doctor is cool, most likely, it is so. And then either his administration starts working according to the existing rules, or he changes the hospital. If we say that we trust only these two teams and send everyone there, we will never meet the need for transplants in Ukraine."

